Look What I Did, Honey
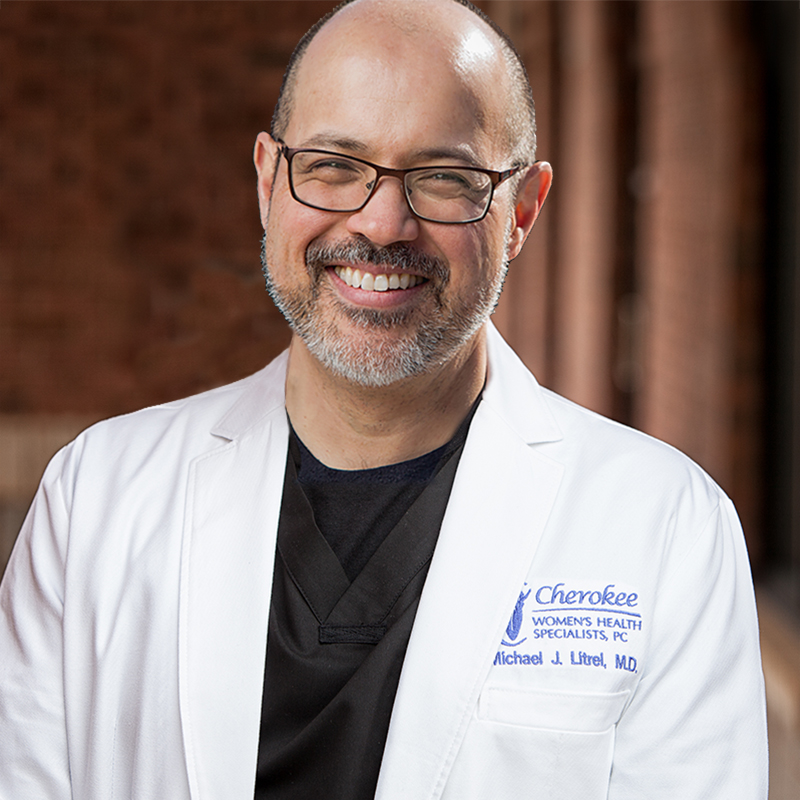
By Michael Litrel, MD, FACOG, FPMRS I usually ask the father to cut the umbilical cord when he’s at the delivery. It’s not that I need the help. Rather, cutting the cord is an important symbolic event. An expectant woman becomes a mother, a family is born, hope wonderfully fulfilled. But there’s another reason to involve the father. Fathers can be pretty useless at times like this. Women understand this sad fact but for the most part keep it secret from us men. A man’s ego is a fragile thing. We’ve convinced ourselves we’re strong and smart and in command. But as we bear witness to the awesome struggle of a woman’s labor, even the most dim-witted of us begin to suspect something is up. The moment the baby is born and new life is miraculously brought forth, we begin to understand the errors of our thinking. It’s a life-changing experience – the realization of the true beauty of the mothers of our children. We are humbled. But we men don’t handle being humbled very well. We confuse humility with humiliation. A new mother’s life is difficult enough without having her husband’s damaged ego to nurse as well as her baby. With this in mind, I’ve found it useful to distract the husband with an accomplishment of his own so the mother’s postpartum course is not unduly burdened. So, he gets to cut the cord. Cutting the cord is technically less difficult than cutting coupons out of the Sunday paper. Most men realize this, and although very well satisfied with their small contribution, keep their self-congratulations to a minimum: “Sweetheart, with you carrying the baby for nine months, and all those painful contractions and pushing, and me cutting the cord so well, I think we both did a pretty good job.” Yet the occasional father takes it to the extreme. “Look what I did, honey!” He looks to his wife, exhausted from her labor and blood loss, for approval. “Did you see me? I just cut the cord! By myself!” Chest swelled with pride and beer belly drooping over his belt, this is the kind of man who walks around for the next couple of decades completely self-satisfied with the thought “that thing would still be attached to you if it wasn’t for me.” Some husbands, on the other hand, are appropriately appreciative. One of these appreciative husbands came to my office with his wife every visit. They had already tried for several years without success to conceive and suffered tremendously from a sense of failure and loss of hope. They submitted to the usual battery of tests in the painstaking task of attempting to time the miracle of conception. After several months with no success, we were considering a reproductive endocrinologist but then out of the blue my patient conceived. Throughout the next nine months, her husband was an unfailing source of support and encouragement. On the day of the delivery he was beside his wife, holding her hand, from the moment of her first contraction. “You are so beautiful!” he told her. “You are doing so well!” Throughout her long labor he rubbed her back, he hugged her, he got her sips of water. And again and again he repeated his mantra – “you are so beautiful, you are doing so well.” Finally the baby emerged. The father’s hand trembled as he cut the cord, and when I placed the baby on the mother’s abdomen, he began to weep uncontrollably. I watched as he hugged his wife and newborn daughter, and at that moment, as the family began their new story, all the self-doubts and suffering of the past seemed to evaporate in an instant into an indescribable joy. It shone from their faces through their tears. And the room could hardly contain it. “You are both so beautiful,” he told his family, his voice cracking. Their past trials hadn’t darkened their happiness, but like a piercing light, had made their happiness more clear. Unlike the quick snip of a cord, with its illusion of accomplishment, the suffering they had borne for so long had opened their eyes, so they could see their child for the miracle she was. I think this is true for all of us. The burden of pain that accompanies us throughout our lives can sometimes be life’s most mysterious gift as well. It strengthens our vision, so we can recognize the miracle of joy that often waits for us, just on the other side of despair.