5 Symptoms Women Should Never Ignore – and Why You Should See Your OB/GYN ASAP
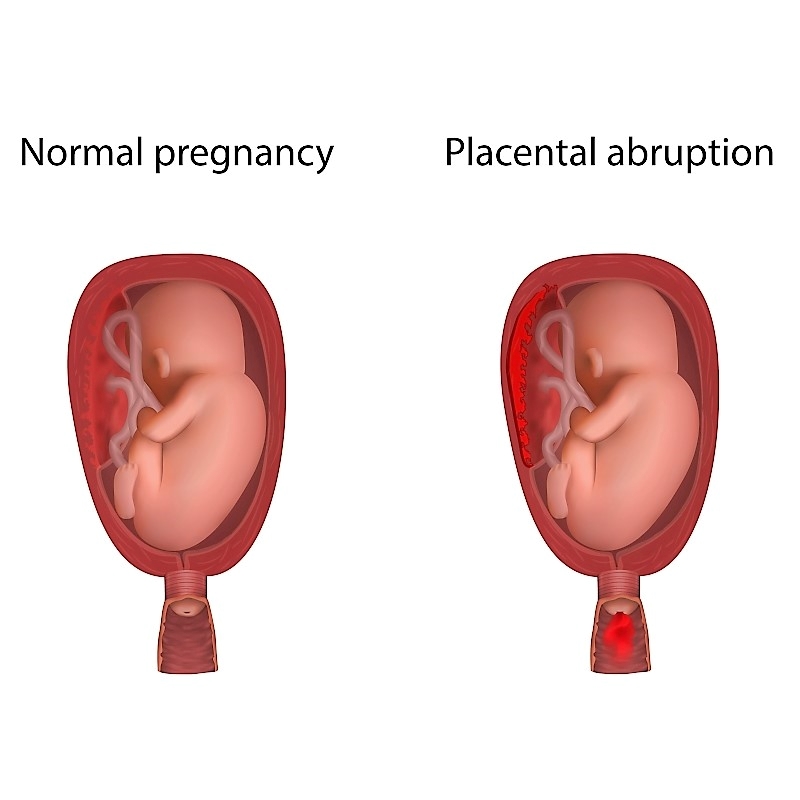
There are five health symptoms women should never ignore and as OB/GYNs, we have seen many cases where women have waited too long to take care of their own health problems, and often regret it later after a bad diagnosis. Do not let this happen to you. Following are five of the most concerning women’s health problems that you should never neglect. If you have any of these five symptoms, make an appointment with your OB/GYN as soon as possible. 5 Symptoms You Should Never Ignore 1. Heavy or Painful Periods When it comes to your periods, you know what’s normal for you. If you experience heavy or painful periods that are out of the ordinary, you need to be seen by an OB/GYN. These symptoms can signal gynecological problems that need treatment. Some could be very serious, such as cancer, but many women have noncancerous uterine fibroids or tumors that cause heavy or painful periods. There are treatments available for uterine fibroids and other gynecological problems known to cause heavy or painful periods. 2. Abnormal Vaginal Bleeding If you experience bleeding between periods or bleeding after menopause, see your OB/GYN. Although abnormal bleeding can occur for many different reasons, gynecological cancers like cervical or uterine cancer are among them. Endometrial hyperplasia happens when the uterine lining grows thick, and is a noncancerous cause of abnormal bleeding. Abnormal vaginal bleeding is what it sounds like – abnormal – and is nothing to take lightly. See your doctor ASAP for treatment or to rule out anything concerning. 3. Pain During Sex Pain during sex can be caused by many different issues. A serious medical condition would need to be ruled out. It also could be endometriosis, which can even lead to infertility. Endometriosis is when tissue similar to the lining of the uterus starts to grow outside of the uterus. In addition to painful intercourse, watch for pelvic pain, extremely painful periods, and pain when you go to the bathroom. There are treatment options available, but you need to know what is going on with your body to be proactive. 4. Lumps in or Around the Breast Regular mammograms and self-breast exams are a must. Do not put off getting regular mammograms and see your OB/GYN at least once a year for evaluation. With no family history, mammograms should begin for every woman at age 40. If there is a family history of breast cancer, your OB/GYN may recommend you start getting mammograms earlier. If you notice anything unusual or different during a self-breast exam, in your breast, around your breast, or under your arm, see your doctor immediately. As OB/GYNs treating thousands of women over the years, we have diagnosed breast cancer in all ages and types of women, even if it there is no family history. The earlier you are diagnosed, the better your prognosis may be so do not delay seeing your OB/GYN or regular mammograms – ever. 5. Nipple Discharge It’s extremely important to pay attention to your breasts. In addition to checking for lumps or changes in breast size or shape, watch for nipple discharge. Discharge, especially bloody or clear discharge, can be a sign of breast cancer. Don’t put off getting checked by an experienced OB/GYN who can properly evaluate you and order the appropriate images and tests. Listen to Your Body If you have symptoms that are not typical for you, or something doesn’t feel right, listen to your body. You know your body best and can sense when something may be wrong. Seeking treatment early can help ensure the best outcome possible. Make taking care of yourself a priority. You are too valuable to neglect. Make an Appointment Today Our board-certified OB/GYNs are here for you. Call us at 770.720.7733 or schedule an appointment online to make an annual exam appointment or to discuss any issues of concern.